Jessica Riggleman, Owner of Raeco, LLC, examines the global regulatory landscape for psychedelic drugs, with a particular focus on Schedule I classification
Depending on the country and specific drug, the global regulatory landscape for psychedelic drugs is complex and variable. Generally, most countries regulate psychedelic drugs as controlled substances, with varying degrees of legal and medical restrictions on their use, possession, and distribution.
Canada
Psychedelic drugs are regulated under Canada’s Controlled Drugs and Substances Act, which restricts their use, possession, and distribution. However, Health Canada has recently begun to grant exemptions for using psilocybin in end-of-life care and research purposes.
Europe & The United Kingdom
In Europe, the regulatory landscape for psychedelic drugs varies by country.
In the Netherlands, for example, some psychedelic mushrooms are legal to possess and use under certain circumstances. In most other countries, they are regulated as controlled substances. In the United Kingdom, psilocybin is a Schedule I drug, although there are growing calls for its reclassification to allow for therapeutic use.
South America
In South America, traditional indigenous use of psychedelic plants such as ayahuasca is legal and widely practiced, although the use of these substances outside of traditional contexts is typically prohibited.
The United States
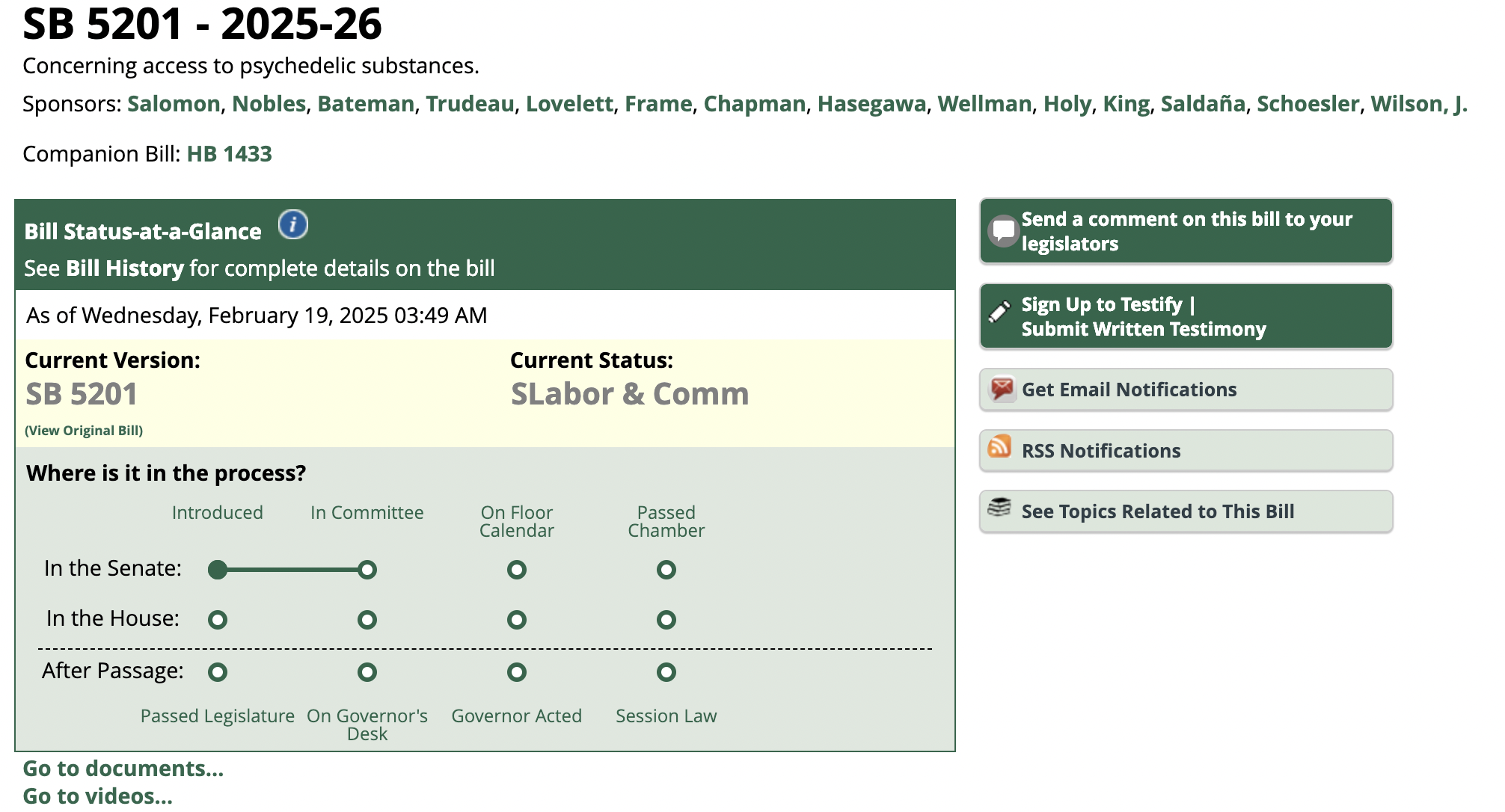
Psychedelic drugs such as lysergic acid diethylamide (LSD), psilocybin, and 3,4 Methylenedioxymethamphetamine (MDMA) are classified as Schedule I substances under the Controlled Substances Act, indicating that they have a high potential for abuse and no accepted medical use. However, some states have recently passed laws allowing for the therapeutic use of these drugs under certain circumstances.
Deep Dive into psychedelic regulation: Schedule I classification
Overall, the global regulatory landscape for psychedelic drugs is complex and evolving, with increasing recognition of their potential therapeutic benefits and growing calls for their reclassification and increased access for medical and research purposes. However, significant legal and regulatory barriers remain, particularly in countries where these drugs are classified as Schedule I substances with no accepted medical use.
The U.S. Food and Drug Administration (FDA) has not approved any psychedelic drugs for therapeutic use except for ketamine, which is approved for treatment-resistant depression. Ketamine is often classified as a dissociative anesthetic, rather than a classical psychedelic like LSD or psilocybin. However, it does have some psychedelic properties, particularly at higher doses. There has been growing interest in the potential therapeutic benefits of psychedelic drugs such as psilocybin, MDMA, and LSD for various mental health conditions, including depression, anxiety, addiction, and post-traumatic stress disorder.
The FDA regulates drugs based on their intended use, and the approval process typically involves several stages, including preclinical research, clinical trials, and review processes.
For psychedelic drugs, the regulatory pathway is complicated by their Schedule I classification under the Controlled Substances Act, which means that they are considered to have a high potential for abuse and no accepted medical use.
Protecting against the abuse of psychedelic drugs
The potential for abuse of psychedelic drugs is influenced by a number of factors, including the dose, the route of administration, the setting in which the drug is used, and the individual’s past experiences and expectations. In a controlled therapeutic setting, the risk of abuse is generally considered to be low, as the drugs are administered under careful supervision and in a supportive environment.
The Schedule I classification of psychedelic drugs poses significant challenges to their development and research as potential therapeutics. The Controlled Substances Act of 1970 classifies Schedule I drugs as substances with a high potential for abuse, no accepted medical use, and a lack of accepted safety for use under medical supervision. This classification imposes several restrictions and barriers to the development of psychedelic drugs as therapeutics.
The Schedule I classification restricts the availability of these drugs for research purposes. Researchers must apply for a special license from the Drug Enforcement Administration (DEA) to conduct studies with Schedule I drugs, and the application process can be lengthy and cumbersome. This creates a significant barrier to entry for researchers who want to study the therapeutic potential of these drugs.
There is limited funding available for research into these drugs. Some government agencies are generally prohibited from funding research into Schedule I drugs, which limits the available resources for studying their potential therapeutic effects.
This classification imposes additional regulatory requirements on drug developers who want to bring psychedelic drugs to market as therapeutics. The FDA requires a higher level of evidence for drugs in Schedule I compared to those in other schedules, which can make the approval process more difficult and time-consuming.
Schedule I classification closing thoughts on the regulatory landscape for psychedelic drugs
Finally, the Schedule I classification carries a significant stigma and cultural baggage, which can make it more difficult to conduct research and bring these drugs to market. Many people still associate psychedelic drugs with the counterculture of the 1960s and 1970s and view them as dangerous and potentially harmful.
Read full article at https://www.openaccessgovernment.org/article/the-global-regulatory-landscape-for-psychedelic-drugs/155963/


 Cannabis News2 years ago
Cannabis News2 years ago
 One-Hit Wonders2 years ago
One-Hit Wonders2 years ago
 Cannabis 1012 years ago
Cannabis 1012 years ago
 drug testing1 year ago
drug testing1 year ago
 Education2 years ago
Education2 years ago
 Cannabis2 years ago
Cannabis2 years ago
 Marijuana Business Daily2 years ago
Marijuana Business Daily2 years ago
 California2 years ago
California2 years ago