Psychedelic Health UK report
In what marks an important development for Europe, a number of EU bodies have published a joint commentary in the world-leading medical journal, The Lancet, acknowledging the therapeutic potential of psychedelics.
The European Medicines Agency (EMA), experts from the EU regulatory network and representatives from the European College of Neuropsychopharmacology (ECNP) have jointly issued the commentary.
Entitled ‘The Therapeutic Potential of Psychedelics: The European Regulatory Perspective’, the commentary explores classic psychedelics specifically – mescaline, DMT, LSD and psilocybin – as potential treatments for mental health conditions.
See also PAREA 2023: campaigning for psychedelic therapy in Europe
The authors highlight that, with mental health problems affecting more than one in six people, this brings considerable economic costs that exceed 4% of gross domestic product across the EU. In this regard, they emphasise the need for effective and safe new treatments for mental disorders.
Exploring a number of challenges that will need to be addressed, the authors raise issues informed by work for the EMA, the EMA’s Central Nervous System Working Party and the ECNP.
See also Discussing Alberta’s move to regulate psychedelic therapy
The Psychedelic Access and Research European Alliance (PAREA) has welcomed the development, which it describes as an “opportunity to open up an institutional debate about moving towards safe, effective and accessible adoption of psychedelic-assisted therapies in Europe.”
Research and clinical trials
Some of the key issues addressed by the authors include challenges with research methodology to enable valid efficacy estimations in clinical trials.
The authors cover double blinding, the roles of positive and negative expectancy, and the use of independent, blinded external raters (including psychedelic naive patients).
Additionally, the need for investigation to establish optimum doses of psychedelics and individualised dosing, along with the relation between characteristics of the acute psychedelic experience and clinical improvement, are highlighted.
Regarding psychedelic-assisted psychotherapies, the authors note the need for trials to establish the added value of psychedelics compared with psychotherapy or psychological support alone, and that preparatory psychotherapy sessions should be investigated.
Barriers to research in Europe
Classic psychedelics all sit in Schedule 1 of the UN’s Convention on Psychotropic Substances of 1971, meaning it is currently extremely difficult to carry out research into the substances due to the costs associated with licensing.
The authors highlight this as another issue that needs to be addressed, suggesting that the UN’s classification of the substances may need to change due to their potential as a therapeutic, along with the fact that they do not show potential for addiction – one of the criteria a substance must meet to be classified in Schedule 1 of the Convention.
The authors state: “Classic psychedelics do not show potential for addiction and the justification for the UN schedule 1 classification (ie, drugs with “no currently accepted medical use and a high potential for abuse”), as adopted in the 1971 Convention on Psychotropic Substances, should be questioned by evidence of the therapeutic potential of psychedelics.”
Tadeusz Hawrot, Founder and Executive Director of PAREA, told Psychedelic Health: “The most restrictive scheduling of psychedelic compounds directly contributed to and reinforced a long scientific stagnation by detracting scientists from conducting research in this area.
“Likewise, European governments and EU bodies have been discouraged from supporting psychedelics research. This lack of public funding has been further undermining the ability to pursue psychedelics research, especially for those scientists who are less resourced and are not affiliated with the industry.
“Consequently, companies and private donors typically fund psychedelic trials and the regulatory constraints and patent incentives create a pharmaceutical landscape that privileges high-cost synthetic variants over existing substances.
“Relying predominantly on industry-supported research to achieve the regulatory approval is not an equitable solution to rescheduling psychedelics with medicinal properties and yet, currently approval of scheduled medicines (by regulators such as EMA) and rescheduling are effectively synonymous.
“Psychedelics should have their classifications reviewed based on the recent scientific and medical progress, independent of their possible regulatory approval as medicines. The support from The Lancet commentary authors in this regard is much welcome.”
Regulating psychedelic therapy
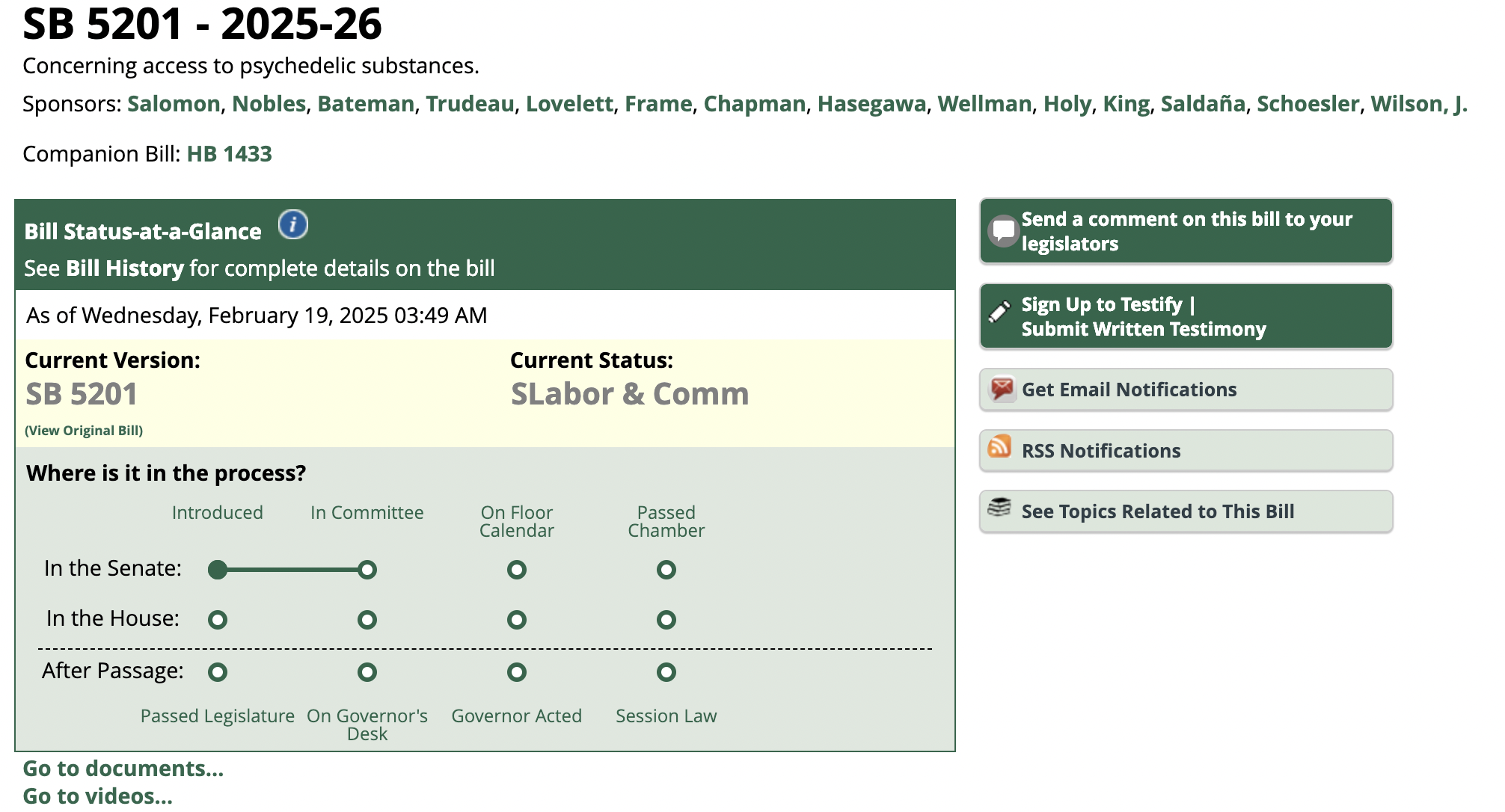
As symbolised by recent developments – such as Australia’s rescheduling of MDMA and psilocybin for depression and PTSD, Canada’s inclusion of the latter on its Special Access Programme (SAP) and Colorado and Alberta’s moves to decriminalise psychedelics – the need to address regulation around psychedelics is becoming increasingly important.
Under Australia’s new approach, any psychiatrist looking to prescribe psychedelic therapies will need to be approved under the Authorised Prescriber Scheme by the TGA following approval by a human research ethics committee.
In their Lancet commentary, the authors stipulate that given approval, regulation around psychedelics in Europe should see conditions and restrictions related to safe and effective use defined at the time of approval, and monitoring requirements in place before, during, and after administration of the substances.
Regulatory tools that could facilitate this include product characteristics, risk management plans and pharmacovigilance studies, along with educational materials, appropriate training and controlled access programmes.
The authors conclude: “The therapeutic potential of psychedelics has triggered new hopes and high expectations, but larger clinical trials are needed to further evaluate efficacy and safety.
“A thorough scientific assessment of the benefit–risk balance will be required, as for any other medicines.
“Developers are encouraged to engage early with the EMA through all available scientific and regulatory platforms in their efforts to overcome the challenges associated with the development of psychedelic treatments.”
Source: https://psychedelichealth.co.uk/2023/02/15/eu-bodies-perspective-regulation-psychedelics/


 Cannabis News2 years ago
Cannabis News2 years ago
 One-Hit Wonders2 years ago
One-Hit Wonders2 years ago
 Cannabis 1012 years ago
Cannabis 1012 years ago
 drug testing1 year ago
drug testing1 year ago
 Education2 years ago
Education2 years ago
 Cannabis2 years ago
Cannabis2 years ago
 Marijuana Business Daily2 years ago
Marijuana Business Daily2 years ago
 California2 years ago
California2 years ago