By: Juan Sebastian Chaves Gil
The increase of sales and free consumption of marijuana on the streets of Europe is becoming more and more evident. In countries like Spain, the consumption of marijuana is no longer considered a taboo by the population. In this European country, there are no regulations prohibiting the cultivation of marijuana, and there are no minimum or maximum limits for the possession of personal cannabis cultivation in a home or private property.
The expansion of cannabis cultivation, marketing and distribution internationally is driven by a variety of motivations. Each nation has its own regulations, which vary according to the intent of the user and other factors such as medical, scientific or recreational use.
In the European Union, there is no uniform regulation of cannabis use. Over the past two decades, there has been a trend to reduce or eliminate prison sentences for possession of small amounts of this substance. In addition to Germany, several other countries have introduced, or are considering introducing, new regulations allowing the recreational use of cannabis.
Frank Perit, a regular cannabis user, welcomes initiatives in Europe that allow the free consumption of cannabis in public spaces. Compared to Latin American countries such as Colombia, where the consumption of cannabis in public spaces can be complicated by the persistence of taboos and legal restrictions, “there is still a taboo on this plant, not to mention that the country is a producer of it on a medical level but not on a recreational level, so to see that Europe does not have this issue is wonderful,” Perit explained. He appreciates the European perspective.
Germany one step closer to legalization
Germany is taking a step toward legalization. A few months ago, the country prepared a law to legalize cannabis, at least partially. Under the law, which will take effect in 2021, adults will be able to possess up to 7 grams of cannabis and grow up to four plants in their homes. The bill to decriminalize cannabis in Germany is expected to take effect no later than January 1, 2024, which is a significant step forward.
Several European countries have adopted more flexible measures, while others are considering amending their regulations to allow consumption in designated public places. Over the past two decades, there has been a marked trend toward reducing or eliminating prison sentences for possession of small amounts of prohibited substances. These countries hope that by adopting these new regulations, the illegality and chaos associated with prohibition will be reduced.
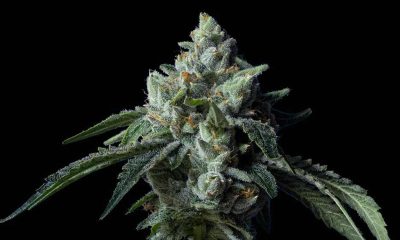
Frank Perit, who has traveled throughout the European continent, believes these measures are a good option. In addition, he highlights the quality of products grown in European countries, such as those of the Amsterdam Marijuana Seeds brand. “They are very reliable, they breed excellent plants like indica and sativa, they create excellent produce and they breed them here in Europe, why not allow more expansion of the product without restrictions, that would seem excellent to me. Frank concludes that Europe is on the right track to expand access to quality cannabis products.
Current state of cannabis in Europe
Several European countries now allow both recreational and medical use of marijuana, setting an encouraging precedent for their neighbors. The Netherlands is known for its liberal approach to cannabis and other drugs. The possession and use of up to five grams of marijuana has been allowed since 1976, and its sale in licensed “coffee shops” is tolerated. However, it is not allowed to grow or sell large quantities. In addition, in 2003 they became the first EU member to allow the medicinal use of cannabis.
Malta has decriminalized the possession of up to seven grams of cannabis and the cultivation of up to four plants by the end of 2021. It also plans to establish licensed Cannabis Social Clubs for the formation of cultivation cooperatives. However, consumption in public places and by minors remains illegal.
Luxembourg has allowed the cultivation and consumption of small amounts of cannabis in private, since June 2023, although carrying more than three grams in public is punishable and considered drug trafficking.
The Czech Republic has had a flexible approach to cannabis since 2010, with possession punishable by law but no legal measures for small amounts. In April 2023, the Czech government plans to legalize cannabis and create cannabis clubs, as well as allow sales in pharmacies.
Switzerland prohibits cannabis, but allows cannabis products with less than one percent THC. It also allows the cultivation of low-THC cannabis strains. As of May 2021, consumers will be able to legally purchase cannabis products in scientific pilot programs under strict conditions in order to obtain a sound scientific basis on the subject.
Marijuana is experiencing a global shift in perception that demonstrates its potential for both health and social benefits. The negative stigma that has persisted over the years is being left behind, and this is producing positive results both economically and clinically.