Husch Blackwell prepared and filed an amicus curiae brief on behalf of nearly 30 end-of-life and palliative care clinicians, urging the U.S. Court of Appeals for the Ninth Circuit to compel the U.S. Drug Enforcement Agency (DEA) to initiate proceedings that could lead to a rescheduling of psilocybin for use in the end-of-life clinical setting.
The amici support the position of Seattle-based physician Sunil Aggarwal, who has been embroiled in long-running litigation with the DEA over the use of psilocybin. Following administrative law procedure, Dr. Aggarwal had asked the DEA to render an opinion on the use of psilocybin—currently a Schedule I drug—for palliative-care patients in light of the federal Right to Try (RTT) Act, passed in 2018, that allows certain patients access to investigational drugs outside of clinical trials. The Food & Drug Administration (FDA) defines Schedule I drugs as those “with no currently accepted medical use and a high potential for abuse.”
In the initial suit, the DEA refused to allow the use of psilocybin under RTT or otherwise condone its use outside of clinical trials, despite the fact that psilocybin has twice been designated by the FDA as a breakthrough therapy, arguably making it eligible for use under RTT laws.
Dr. Aggarwal’s initial efforts ended without a ruling on the merits of the case itself. The Ninth Circuit determined in January 2022 that it lacked jurisdiction to review the matter because the DEA had not yet issued a final agency decision. This ruling touched off a series of back-and-forth administrative law procedures that resulted in Dr. Aggarwal filing a citizen petition directed at the rescheduling of psilocybin itself, rather than the DEA’s regulatory posture toward psilocybin in light of the RTT Act. Dr. Aggarwal’s rescheduling petition was summarily rejected by the DEA in September 2022, leading to the current Ninth Circuit appeal.
In addition to the clinician signatories on the Husch Blackwell-authored brief, there are multiple groups supporting Dr. Aggarwal’s appeal, including medical researchers, professors of law, state legislators, and veterans’ affairs advocates. Additionally, policy institutes spanning the political spectrum, including the Goldwater Institute and the Cato Institute, have endorsed Dr. Aggarwal’s position in a bipartisan show of support.
Dr. Aggarwal and the Advanced Integrative Medical Science Institute—of which Dr. Aggarwal is a co-director—is represented by Shane Pennington of Vicente Sederberg LLP, Matthew C. Zorn of Yetter Coleman LLP, Kathryn L. Tucker of the National Psychedelics Association, and James F. Williams, Thomas J. Tobin, Andrew J. Kline, and Holly Martinez of Perkins Coie LLP.
“We are so grateful to see so many prominent hospice and palliative care clinicians support Petitioners in this important case,” said Tucker. “These clinicians know the suffering their patients endure with unrelieved anxiety and depression and are eager to add psilocybin-assisted therapy to the palliative care toolbox as soon as possible, because it brings immediate, substantial and sustained relief.”
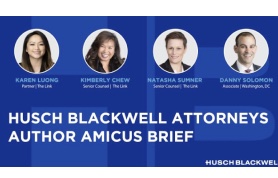
“This case is, appropriately, centered on issues of administrative law, but the amici want to remind the court that there is so much more at stake,” said Husch Blackwell partner Karen Luong. “This is about basic human dignity, recognition of the medicinal use of psilocybin, and the right of dying patients to access valuable therapies that might help them in their last days. The DEA’s action has muzzled the most important voices in this fight—the doctors on the front lines and the patients themselves. We are honored to help these voices be heard.”
The Husch Blackwell team included Luong, Kimberly Chew, Natasha Sumner and Danny Solomon.

 Cannabis News1 year ago
Cannabis News1 year ago
 One-Hit Wonders1 year ago
One-Hit Wonders1 year ago
 Cannabis 1011 year ago
Cannabis 1011 year ago
 drug testing7 months ago
drug testing7 months ago
 Marijuana Business Daily1 year ago
Marijuana Business Daily1 year ago
 Education1 year ago
Education1 year ago
 Cannabis1 year ago
Cannabis1 year ago
 Education1 year ago
Education1 year ago
















