Emotional
How Do Psychedelics Change Our Thoughts on Death?
Published
9 months agoon
By
admin
A recent study undertook the question of how psychedelics change our thoughts on death; in comparison to near-death experiences, and other irregular experiences. What did the study find regarding our changing attitudes about death and dying? Read on for more information.
Study on psychedelics effect on feelings about death and dying
The study, entitled, Comparison of psychedelic and near-death or other non-ordinary experiences in changing attitudes about death and dying, looks at several different scenarios, and how they effect our thoughts on death and dying; as well as to gauge which specific psychedelic drugs caused the greatest change in these thoughts.
According to study authors, “Both psychedelic drug experiences and near-death experiences can occasion changes in perspectives on death and dying, but there have been few direct comparisons of these phenomena. This study directly compared psychedelic occasioned and non-drug experiences which altered individuals’ beliefs about death.”
The study used 3,192 participants, split into five groups. These groups were: 1) those who had a near-death or irregular experience without use of a drug (933 participants); and those who had a near-death or irregular experience using psychedelics, with 904 in the LSD group (group 2), 766 in the psilocybin group (group 3), 282 for ayahuasca (group 4), and 307 in the group that did a non-ayahuasca form of DMT (group 5).
How the study was done
The participants were recruited in different ways over the internet; including through a newsletter, email invitation, blog post, social media post, or advertisement. The participants took one of two surveys. Th first was geared toward near-death experiences, but which also included other irregular experiences like feeling out-of-body. The second survey was about psychedelic experiences. The surveys were hosted on www.qualtrics.com, with appropriate links per survey. Each participant gave consent on the first page of the survey.
On this consent page, investigators listed the purpose of the study, for the participants to understand what they were giving information for. It read, “to characterize an experience that fundamentally altered your beliefs or understanding about death and dying.”
Participants were put in the Psychedelics Group, if they filled out a survey based on taking a classic psychedelic drug: LSD, psilocybin (magic mushrooms), or DMT (whether ayahuasca, or just DMT). The Non-Drug Group completed their own survey about a near-death experience, or some other irregular occurrence. Completion of the survey was required for entry, and all participants remained anonymous. No participants received any compensation for participation. The Johns Hopkins University School of Medicine Institutional Review Board, approved study procedures.
The surveys used multiple choice questions and open-ended fill-in questions, to gain information on the experiences. In the Psychedelic group, questions were included about length of experience, if there was a threat to life, how it happened, and what it was like. Study subjects filled-out an assessment of what they experienced, and how it affected them, using the Greyson Near-Death Experience (NDE) Scale.
This included subscales for ‘cognitive’ effects, ‘affective’ effects, ‘paranormal’ effects, and ‘transcendental’ effects. The Hallucinogen Rating Scale (HRS) was used to evaluate subjective details and any life change associated with the experience. Investigators also used the following assessment tools: States of Consciousness Questionnaire, the Persisting Effects Questionnaire, and the Mystical Experience Questionnaire.
These were accompanied by a single question “During your experience, did you encounter something that someone might call ‘God’”. Participants then filled out the Revised Death Attitude Profile, to evaluate how their views changed pre and post experience; and the DAP-R, which included subscales for ‘fear of death,’ ‘death avoidance,’ ‘neutral acceptance,’ ‘approach acceptance,’ and ‘escape acceptance.’

Study results for how psychedelics affect thoughts on death
This study undertook the question for how psychedelics, and other non-drug near-death experiences, change our way of thinking about death and dying. The results indicate that both circumstances can affect how a person feels. However, the two kinds of experiences led to different results.
The Non-Drug group more often reported that they had been clinically dead, or unconscious; and that they had faced grave danger. However, the groups were very similar in how their feelings changed toward death, based on their experiences. These feelings included a reduction in the fear of death, as well as positive and persistent effects related to the personal meaning of an event, the psychological insight into it, and its spiritual significance.
The study results indicate that though both groups were associated with increases in near-death and mystical experiences; that the Psychedelics group had greater and more significant results. The Non-Drug grouping was more likely to view the experience they had as the absolutely most meaningful experience of their current lives.
In terms of assessing which psychedelics led to the greatest effects on feelings of death and dying, the two DMT groups (DMT and ayahuasca) reported stronger and longer-lasting positive results from their experience, than those who used LSD or magic mushrooms. For the latter two drugs, the results were nearly the same.
How feelings toward dying changed
The study looked at changes in personal perspective on death and dying, following a drug-fueled, or non-drug-fueled near-death or abnormal experience. A change in feelings implies a change in feelings on the topic, but does not indicate directly whether it relates to a positive experience (lessened fear) or negative experience (increased fear).
This study indicates that most go toward the lessened fear end. The results found that 90% said their experience decreased their fear of death and dying. According to study authors, not only did it take away fear for these participants, but the experience often “resulted in positive, desirable changes in their curiosity and attitudes about death, including their own death.”

Researchers found that less than 1 out of 10 participants said they had an increase in fear of death or a negative change in their overall feelings on the matter. This indicates that near-death and other irregular experiences, are more highly correlated with a lessening of fear, than an increase of it; when it comes to personal thoughts on death and dying.
Psychedelics for end-of-life care
Though this might be one of the first studies formally into this concept, the idea that psychedelics can reduce fear and anxiety in end-of-life situations, and in palliative care, is understood. In fact, its so well understood, that this is often the reasoning for a push to legalize psychedelic compounds.
End-of-life scenarios usually relate to the end of a sickness, or age-related decline. Palliative care refers to the treatment of illnesses that are terminal, or otherwise very serious, and a cause for extreme discomfort to the patient. Psychedelics are already being eyed for their ability to aid in the fear and anxiety associated with dying, in these populations.
Right now, though this idea has grown more prevalent, there are few-if-any current exemptions for this purpose. But it is being studied. In 2022, we reported that British start-up Clerkenwell was scheduled to begin trials into the use of psilocybin for those with terminal diagnoses or undergoing palliative care.
It’s not surprising that psychedelics can be used in this way, as its becoming more and more understood the part these drugs can play in PTSD, another ailment related to fear. Not only have fMRI and EEG studies shown a lessened fear response in relation to use of drugs like DMT and MDMA; but the organization MAPS already received a ‘breakthrough therapy’ designation for its MDMA PTSD drug; Colorado already legalized the compound for medical purposes, contingent on a federal approval; and Australia recently became the first country to approve MDMA for medical use.
Conclusion
We also currently have an industry of ketamine clinics in the US related to helping people with all kinds of mental health issues, including anxiety. And an incredible amount of research into multiple psychedelic, and non-psychedelic hallucinogens, for a plethora of psychiatric purposes. This new research into how psychedelics can mitigate fear of death and dying, helps expand out knowledge on the uses of these compounds.
Welcome all! We at Cannadelics.com, appreciate your visit. We’re a hard-working team, here daily to bring you the best in reporting for the cannabis and hallucinogen spaces. Visit us frequently to stay up-to-date on important happenings, and check out the Cannadelics Weekly Newsletter; so you’re always up on what’s going down.
Related
You may like
channa
Kanna – What It Is, And How It Can Help You
Published
3 months agoon
January 21, 2024By
admin
The world of natural medicine is full of plants to promote wellness; here’s a little on kanna, and what it can do for you.
What is kanna?
At first glance, it might look like this is a shortened version of ‘cannabis’, spelled with a ‘k’ rather than a ‘c’. If you say it out loud it also sounds like you’re right about to say ‘cannabis.’ In reality, the two plants have very little in common except a name that sounds a bit similar.
Kanna is technically named Mesembryanthemum tortuosum, or Sceletium tortuosum, which are both obviously quite a mouthful. It also goes by the nicknames channa, and kougoed; the latter of which translates to ‘something to chew.’ It’s a succulent plant that hails from South Africa, particularly the Cape Provinces, where it was used primarily by the San and Khoikhoi peoples. It’s in the Aizoaceae family of plants.
The plant has small full leaves (as it is a succulent), and yellow and white flowers. The flowers are more yellow in the center and white around the outsides; and the petals are long and thin, and resemble spears shooting out from the center.

The plant has been used in South Africa since pre-historic times, or at the very least, a super long time. It wasn’t written about formally until 1662, when Dutch navigator Jan van Riebeeck first mentioned something about its use. The plant is usually dried and then chewed; although it can be made into a tea, or a snuff to smoke. In modern times, it’s often seen as a capsule, powder, or tincture, as well.
Traditionally, the plant was/is used to deal with issues like stress, and depression. Native cultures use it to promote relaxation and general wellbeing. It was/is also used as a pain medication, and as a way to suppress the appetite. Furthermore, it’s been studied for its ability to help dogs and cats which are suffering from dementia, from barking or meowing excessively at night.
Is kanna psychoactive?
Oftentimes, a plant’s name is derived from a major (or important) component within it. Such is the case for Mesembryanthemum tortuosum, which contains the active compound mesembrine. Mesembrine is an alkaloid, with about .3% in the roots of the plant, and .86% in the leaves, stems, and flowers.
In research, this compound shows the ability to work as a serotonin reuptake inhibitor. This might sound familiar, as a major class of antidepressant drugs, is called ‘selective serotonin reuptake inhibitors;’ which indicates the plant might have some of the same benefits. Common SSRIs include the heavily prescribed Zoloft and Prozac. As kanna has been used traditionally to combat stress and depression, this connection makes sense. It also makes it a natural version of what pharmaceutical companies produce.
Beyond this, mesembrine has also shown some ability as a weak inhibitor of the enzyme phosphodiesterase 4. Such drugs are associated with memory improvement, anti-inflammatory effects, increased wakefulness, and neuroprotective qualities. They’re thought to be possibly beneficial for a range of disorders, from depression, to Parkinson’s disease and Alzheimer’s disease, to multiple sclerosis, autism, strokes, and more.
All together, this indicates (along with recent research), that mesembrine, and the kanna plant as a whole, might be able to offer some solid benefits in terms of depression and anxiety management, as well as a treatment (whether alone or in conjunction with other compounds) for a range of other neurological impairments, pain issues, and inflammatory problems.

The plant contains another alkaloid called mesembrenone, which is thought to produce similar effects to mesembrine; and which is also thought to promote adaptogenic and antimicrobrial properties. Most plants that cause psychoactive effects (or really any medical effect), generally do so as a combination of compounds, not just one. In the world of cannabis, we specifically call this the entourage effect, but in general medicine its known as a synergistic effect.
What about pain?
Right now, pain is a particularly big topic in the US, as the desire to reduce it, led to what is one of the worst drug epidemics (essentially the worst) to befall civilization. Opioids certainly have a large recreational-only following, but they’re primarily pain medications. And it was their prescription for pain, that led to the mess we’re in. As such, pretty much anything that can help the pain issue, without causing the same problems of addiction, is greatly needed.
Another interesting compound in the plant is mesembrenol. This compound is associated with analgesic (pain-relieving) properties. Both this compound and mesembrine are thought to aid in pain reduction; and with none of the addictive side effects as synthetic opioid medications.
Traditionally, these pain-killing benefits were used mainly by native South Africans to treat headache pressure, abdominal pain, toothaches, for pain in the respiratory tract, and as a local anesthetic. In 2014 mesembrine’s analgesic properties were tested in rats, which were given up to 5000 mg/kg per day, with no adverse reactions. Investigators concluded that mesembrine “appears to have analgesic properties without abuse liabilities or ataxia.”
Human research into kanna safety
Before the rat study in 2014, a study came out in 2013, which investigated how safe and tolerable two different doses of kanna are for humans. The study, called A Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Trial of Extract Sceletium tortuosum (Zembrin) in Healthy Adults used doses of 8mg and 25mg, which were given to participants once a day. The study lasted three months, and used all healthy adults. 37 people participated in the study.
The investigation was a randomized, double-blind, parallel-group, placebo-controlled, single center study. Let’s break this down. First off, there was a placebo group, which means some participants were given the kanna, and some were given an inactive compound. The randomized part means participants were randomly picked for the kanna or placebo groupings; and the double-blind part means neither the researchers nor participants knew which group they were in.

In terms of the parallel group part, this refers to some in the kanna group getting a smaller dose, and some getting a bigger dose; and that individual participants were given the same amount throughout the study. The last part, single center, refers to the study being conducted in only one location. 12 participants received 8mg kanna daily, 12 received 25 mg kanna daily, and 13 received the placebo daily.
Researchers found both doses of kanna to be tolerable. The most complained about adverse response was headache, followed by abdominal pain, and infections in the upper respiratory tract. However, more complaints came from the placebo group than either kanna group; indicating the complaints had little-to-nothing to do with the kanna.
In terms of unsolicited positive benefits (written in the journals of some participants taking kanna), these indicate increased feelings of wellbeing, and an improved ability to manage stress and sleep. As the study didn’t technically look into the effects or benefits of the drug, these unsolicited journal responses are the most that the study can show on the therapeutic front. Otherwise, it was mainly to assess safety and tolerability.
In terms of other physiological aspects, the kanna groups showed no difference in ECG, body weight, or in their physical examinations, which were all taken in the beginning and the end of the study. There were also no changes in hematology or biochemistry metrics, indicating the drug did little to change the body physiologically. Overall, kanna showed to be a physically safe drug at doses up to 25mg a day, regardless of therapeutic ability.
Conclusion
Kanna seems to offer a multitude of benefits to humans, like help with stress and depression, assisting in pain management, anti-inflammation benefits, and as an anti-microbial. Perhaps in the future we’ll see more of it; and perhaps big pharma will ensure that never happens.
Luckily, for those in the US who want to use this plant to help with a mental or physical issue, kanna, and its compounds, are currently perfectly legal. It can already be found in smart shops around the country; and as with anything else, interested users, should go at it responsibly.
Welcome wellness fans! Thanks for dropping by Cannadelics.com, where we cover the most interesting stories in the general wellness space. Stop by regularly to stay up on stories; and check out our Cannadelics Weekly Newsletter, for an assortment of awesome product promotions, as well.
Related
Emotional
Does Topical Ketamine Work? – Cannadelics
Published
4 months agoon
January 12, 2024By
admin
Ketamine can be taken intravenously, via IM, by mouth, by nose (snorted), and even as a topical treatment. How well does this last option work? Read on.
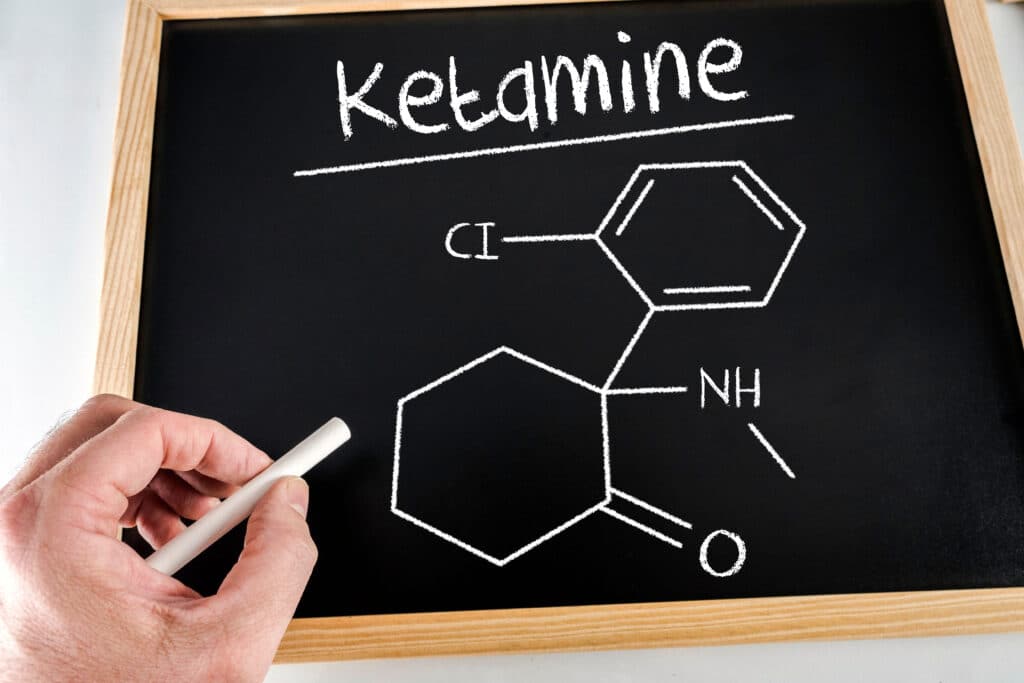
Ketamine basics
Ketamine isn’t a natural compound, but rather, a lab-made drug that was created in 1962 by pharmaceutical company Parke-Davis. In 1970 it received authorization by the US’s FDA as a Schedule III anesthetic for both humans and animals. Ketamine is different from other hallucinogens we speak about, because its actually legal for medical use. We are not talking about a Schedule I drug.
Besides its capability as an anesthetic, which is used for surgery, the drug also shows ability for cataleptic and analgesic effects. Though it causes sedation in users, its not actually a hypnotic, meaning, it doesn’t put a person to sleep. It also doesn’t cause a lowering of vital signs like blood pressure or respiration rate at general anesthetic levels, meaning its quite safe in terms of overdosing.
When ketamine was first tested back in the 1960’s, it was used on a prisoner population. At that time it was established that ketamine had both pain-relieving properties, and some kind of ability to affect mood. In terms of the first point, it went on to be used on the fields of Vietnam. In terms of the second, its been the center of a therapeutic market for several years as an alternative to standard antidepressants for mental health issues. Yet, somehow, there is no further official clearance given for these uses.
Even so, ketamine is used for both. Its legal status opens up a loophole, in that doctor’s can prescribe it for off label uses, if they think the medicine is applicable for the patient. This has led to a large gray market ketamine industry that functions outside the regular medical system. As of yet, there has been no catastrophe, or even near-catastrophe, despite smear-campaigns and warnings by the government.
Topical ketamine
Ketamine is known mainly as a drug you snort on the street. It’s powder, like cocaine, and you can make lines in the same way, or take it as a bump off a fingernail. For most people that do ketamine, this is the way they take it in. When used in a medical setting, however, its generally IV, since its usually used for anesthesia. It can also be injected into a muscle (IM), or taken as a pill; which has become big for at-home treatments.
The delivery method which is spoken about the least, is topical ketamine, but this exists as well. This simply means that ketamine is made into a cream, and put on the skin. While we hear about other methods of ketamine use, we rarely hear about this one. However, it exists, and there is some limited research into it, and current research underway.
In this study from 2015, entitled Analgesic effects of topical ketamine, study authors make a few points, like that ketamine is a good option for neuropathic pain and complex regional pain syndrome, since it doesn’t have serious side effects. They point out that clinically significant side effects are incredibly rare, even at high doses.
It seems there are no large scale studies for this, even though ketamine shows as a good (no, great) alternative to opioids, and the addiction and death issues therein. However, in this study of five patients with sympathetically maintained pain, all showed 65-100% reduction in pain scores, compared to pre-treatment levels. This study of 300 emergency room pain patients from 2021 showed that ketamine reduced pain symptoms; although it performed about the same as lidocaine.
In this 2021 review by Frontiers in Science, called Ketamine Use for Cancer and Chronic Pain Management it states, “Ketamine has repetitively been shown to reduce pain scores and subjective measures of pain. While the use of topical ketamine alone does not have strong supporting evidence, its use in multi-agent creams has been effective in some pain conditions.”

Topical ketamine for PTSD
New testing is underway to see if a topical ketamine product can help with psychological issues, like PTSD. In 2023, it was reported in Clinical Trials Arena, that the company Psycheceutical announced the start of Phase I trials into a new topical ketamine drug meant to treat PTSD, with Phase II trials already on the horizon.
The product, called NeuroDirect, is made to target nerve endings in the neck. This is meant it get around the hallucinogenic effects associated with the drug. How well it works to do so, is a big part of the current trials. They’re meant to assess how safe the drug is, how well its tolerated, and the general pharmacokinetics; all after a single dose. Only 24 patients are included in these trials, however, all are healthy patients. No PTSD in this population
This is the first set of trials that look into whether a topical version of ketamine is safe for a consumer population. Prior to these trials, investigators’ pre-clinical observational results, showed that approximately 80% of participants gained a benefit for their PTSD, from the topical ketamine.
So far, the Phase I participants were all successfully dosed, and the dosing was tolerated fine. Should subsequent trials also go well, this new medication would make ketamine administration easier and safer, since it wouldn’t involve directly entering anything into the bloodstream. Oral use is also an option, but is hard to predict outcomes with, as different patients absorb it quite differently.
Psycheceutical’s CEO Chad Harman, had this to say about the undertaking: “With our goal of a non-systemic treatment for PTSD using legal ketamine, we are attempting to pave the way for our future drug candidates to treat other mental health disorders.”
In terms of the intention for Phase II trials, these would revolve around using the NeuroDirect on PTSD patients. As per an announcement in February of last year, the company is looking to enlist 115 study participants with PTSD, to assess how effective the drug is in reducing PTSD symptoms.

Main benefits of topical ketamine
There are several benefits to using a topical version of ketamine over injected versions or oral versions. For one, its easy to use, and requires nothing more than applying to the skin. It’s just as easy to take a pill, of course, but pills come with the detraction of not knowing how a specific person’s body will break it down and respond.
The topical ketamine is put directly on the back of the neck, because this puts it close to the brainstem. Here, a drug can enter the body without going through the blood-brain barrier. This direct approach is meant to bring down unwanted side effects related to nausea, dizziness, or hallucinations. It does not have to be processed through the digestive tract, like a pill does.
Since the drug uses such a direct application, it can be with a low dose, which brings down any risk of addiction. Realistically, ketamine is rarely spoken about as an addictive drug, except when it comes to companies or governments telling you what product to buy. However, if this idea satiates those entities, all the better.
The simple application method means that patients don’t have to be in a hospital setting, and essentially gives another option for at-home ketamine use. It’s hoped this will bring down costs both for individuals and insurance companies; and allow more people access to these treatments.
Conclusion
For whatever reason we don’t see many topical ketamine products; it seems this is about to change. In the next few years, I expect this product will come to market, as well as plenty of others, as ketamine only grows in popularity. Both for pain issues (particularly as a way to avoid opioids) and the treatment of mental health disorders.
Hello all! We welcome you to Cannadelics.com, an independent rag in the wellness space, here with the best stories of today. Come by daily to be a part of everything; and subscribe to the Cannadelics Weekly Newsletter, for all the best news and product promos.
Related
Emotional
Survey: Psychiatrists More Optimistic About Hallucinogen Therapies
Published
6 months agoon
October 24, 2023By
admin
Hallucinogen therapies are gaining a lot of traction with consumers, as well as with psychiatrists; as per the results of a new study.
Study on psychiatrists and hallucinogen therapies – setup
A new study, entitled American Psychiatrists’ Opinions About Classic Hallucinogens and Their Potential Therapeutic Applications: A 7-Year Follow-Up Survey, is a follow-up study to see the changing opinions of psychiatrists toward newer hallucinogen treatments, like psychedelics. It was recently published in Psychedelic Medicine.
The original study on psychiatrists’ opinions toward psychedelic and hallucinogen therapies, was conducted by the same group of researchers, back in 2016. This was before the mass trend toward legalization and decriminalization of these substances; and was even before the bulk of legal cannabis industries opened. It suffices to say that a lot has changed since this time; and this follow-up was meant to see how the changes in the years in between, have affected how those who treat mental disorders, feel about using such therapies.
The study assesses the level of optimism of US psychiatrists, toward using these treatments. The second study looked at the years 2022-2023; the first, at 2016. The same methodology was used for both the first study, and its follow-up. A survey was emailed to 1,000 members of the American Psychiatric Association; who were picked randomly. This included 750 attending psychiatrists, and 250 resident-fellows. For the second survey, this collection took place at the end of 2022 into the beginning of 2023.

Current responses were measured against 2016 responses using a non-parametric trend test. Investigators also used a multivariate logistic regression model to predict agreement with the incorporation of such therapies into respondent practices.
What did the study find?
Not everyone who receives a survey in life, actually fills it out. In this case, 13.1% of those who received the survey, completed it. This made for 131 participants. The respondents for this follow-up were identified as having similar demographics to respondents in the 2016 original survey.
According to study results, 80.9% believed either moderately or strongly, that hallucinogenic treatments are a promising therapeutic measure for several different psychiatric disorders. 60.8% also thought these treatments show promise for those suffering from substance use disorders as well. The latter means an interest in using these drugs for things like alcohol and opioid addiction.
Even greater percentages wanted to see more research into these topics, signaling an interest in them, even if not to the point of fully approving them just yet. 93.9% strongly or moderately desired more research into their use for psychiatric disorders; while 88.6% wanted to see more research concerning research into their use for substance use issues. In terms of federal funding for clinical trials to better understand these topics; 84.7% supported this for psychiatric disorders, while 80.9% did for drug abuse problems.
These numbers show increased optimism for these therapies in comparison to the 2016 survey. They also show a decrease in fears over using these treatments for patients. Results showed that 50.4% showed a moderate to strong desire to include psychedelic and hallucinogenic-assisted therapies into their own practices.
Investigators concluded from the new survey, that “Our data reveal a striking positive shift in attitudes toward the therapeutic potential of hallucinogens among American psychiatrists since 2016, with a majority of responding psychiatrists planning to incorporate hallucinogen-assisted therapy into their practice if regulatory approval is granted.”

Big changes from 2016
When looking at a comparison like this, it’s important to know about the original study. After all, we want to know what this new comparison, is a comparison to. The original study, called A Survey of American Psychiatrists’ Attitudes Toward Classic Hallucinogens, collected data in 2016, but was published in 2018, in The Journal of Nervous and Mental Disease.
At the time of information collection, the idea of hallucinogenic therapies had been reintroduced to society; but was still way far behind our current acceptance level and understanding. There was considerably less recent research on these topics, at the time that the original survey was given out.
This survey was also sent to 1,000 randomly selected members of the American Psychiatric Association; with the same breakdown of resident-fellows (250) and attending psychiatrists (750). One big difference is that the response rate was much higher for the original; with 32.4% filling out the survey. This means 324 respondents, which is way more than the 131 who answered the follow-up.
According to the researchers about this survey, “Respondents tended to perceive hallucinogens as potentially hazardous and appropriately illegal for recreational purposes.” Many fewer saw hallucinogenic therapies as a positive form of psychiatric treatment; amounting to what researchers called a “large minority,” who did express some optimism.
This investigation found that resident-fellows, and male respondents, were more likely to have greater optimism toward using these treatments, and less overall fear; than female respondents and attending psychiatrists. The results also indicate that younger respondents were more positive about these treatments; which might indicate a generational divide when it comes to the acceptance of these therapies. Younger respondents may have experienced less negative jargon surrounding these drugs and their therapeutic uses, than older respondents.
Are hallucinogenic and psychedelic therapies the same?
If you’ll notice, both study titles involve the word ‘hallucinogens,’ not ‘psychedelics.’ However, in a lot of media reporting, its only the term ‘psychedelics,’ that’s used. What’s the difference? The truth is, there is overlap in the meaning of these words; but they do not mean the same thing.

Basically, all psychedelics are hallucinogens, but not all hallucinogens are psychedelics. This automatically means that all psychedelic therapies, are included when looking at hallucinogen treatments; which encompass psilocybin (from magic mushrooms), DMT, mescaline, and LSD. Even MDMA, which is often included in the ‘psychedelics’ category, is technically classified as a ‘psycho-stimulant.’ However, its still relevant to this study, since it’s a hallucinogen. ‘Psychedelics’ is often used as a catch-all phrase these days, to represent hallucinogenic drugs in general.
Psychedelics are one of three main classes of hallucinogens; together with deliriants (like datura or Benadryl), and dissociative (which include ketamine, PCP, and DXM.) They are generally separated by their mode of action in the brain, and the neurotransmitters they affect most. Psychedelics cause the biggest force at serotonin receptors, deliriants do at acetylcholine receptors, and dissociative drugs at NMDA receptors. These are simplifications, as the drugs can affect different parts of the brain; but it gives an idea of the classification breakdown.
Other hallucinogens exist, which are not in these categories. Like MDMA, which for the most part works similarly to psychedelics, but with a greater stimulant effect; salvia, which affects opioid and dopamine receptors; and amanita mushrooms, which have a strong effect at GABA receptors. These are up-and-coming substances, but the plant world offers tons of other compounds; some of the names of which, are barely recognizable to the public. And some, like blue lotus, and ibogaine, which are starting to enter the conversation, too.
Hallucinogen drugs are defined as “psychoactive substances that produce powerful alterations in perception, mood, and various cognitive processes.” A hallucination, is an experience through the senses, of something that is not real, or altered from reality. This means seeing, hearing, smelling, tasting, or feeling something, in a way that is not actually happening. A hallucinogen is any drug from any class, which produces these effects.
Conclusion
Plenty of psychiatrists are still not up for using hallucinogen therapies, like psychedelics, to treat psychiatric issues. And plenty are interested, but want more information. What is most interesting about the current follow-up, is the sheer change in attitude within less than a decade of time. If the increase was so great from 2016 to 2023; it seems quite possible that by 2030, these therapies will be a norm in the psychiatric treatment world.
Welcome one and all; thanks for being a part of Cannadelics.com; where we bring you cutting-edge reporting on the world of drugs at large – with a particular focus on cannabis and hallucinogens. Head our way daily to catch the updates; and sign up to our Cannadelics Weekly Newsletter; so you’re always aware of the biggest stories.
Related

Senate Leadership Pushes End of Federal Prohibition Of Cannabis

Off To The Horse Races With Cannabis

The Future Of Cannabis After Rescheduling

A Happy Hippie’s Journey of Love, Cannabis, and Self-Discovery

But What about the UN Drug Treaties?

The Best Tips To Up Your Intimacy Game While High

What Can Consumers Expect From Marijuana Rescheduling

The Gilded Age Heiress Who Helped The Marijuana Movement

Tips For Your Body After Hours Of Sitting

Why Falling THC Test Results Matter

Distressed Cannabis Business Takeaways – Canna Law Blog™

United States: Alex Malyshev And Melinda Fellner Discuss The Intersection Of Tax And Cannabis In New Video Series – Part VI: Licensing (Video)

Drug Testing for Marijuana – The Joint Blog

What you Need to Know

Cannabis, alcohol firm SNDL loses CA$372.4 million in 2022

NCIA Write About Their Equity Scholarship Program

City Of Oakland Issues RFP For Employee Training Programs

It has been a wild news week – here’s how CBD and weed can help you relax

A new April 20 cannabis contest includes a $40,000 purse

UArizona launches online cannabis compliance online course
Trending
-

 Cannabis News1 year ago
Cannabis News1 year agoDistressed Cannabis Business Takeaways – Canna Law Blog™
-

 One-Hit Wonders1 year ago
One-Hit Wonders1 year agoUnited States: Alex Malyshev And Melinda Fellner Discuss The Intersection Of Tax And Cannabis In New Video Series – Part VI: Licensing (Video)
-

 drug testing4 months ago
drug testing4 months agoDrug Testing for Marijuana – The Joint Blog
-

 Cannabis 1011 year ago
Cannabis 1011 year agoWhat you Need to Know
-

 Marijuana Business Daily1 year ago
Marijuana Business Daily1 year agoCannabis, alcohol firm SNDL loses CA$372.4 million in 2022
-
 Education1 year ago
Education1 year agoNCIA Write About Their Equity Scholarship Program
-
 Education1 year ago
Education1 year agoCity Of Oakland Issues RFP For Employee Training Programs
-

 Cannabis1 year ago
Cannabis1 year agoIt has been a wild news week – here’s how CBD and weed can help you relax



